GM-elog
This is online E log book to discuss our patients health data shared after taking his guardians informed consent form.
I have been given this case to solve in an attempt to understand topic of" patient clinical data analysis" to develop my competency in reading and comprehensing clinical data including history clinical findings
investigations and come with a diagnosis and treatment plan.
Date of Admission:27/07/22
History of past illness:
A 50yr old male ,farmer by occupation came to opd for Deaddiction
Chief complaints
• Generalized weakness since 15days
• Polydipsia
• Polyuria
History of present illness:
• Patient was apparently asymptomatic 1yr back then he was diagnosed to have diabetes at a government camp.
• So then he was given oral antiglycemic drugs ,he used it for 2months and stopped it.
• So, he developed generalized weakness, polydipsia, polyuria.
• Then he visited a private hospital at nakrekal,then was found to have high sugar levels ,since then he was started with insulin,but he was on a irregular medication.
• He was a k/c/o of type 2 diabetes 1year back.
• He was not a k/c/o hypertension, asthma,CAD, epilepsy
Treatment history
• He was on diabetic medication
• No history of use of any other medication
Family history
• There is no significant family history
Personal history
• Mixed diet
• Normal appetite
• Normal bowel movements
• No known allergies
• Adequate sleep
• Habits-
• chronic alcoholic -180ml/day since 30yrs
•Tobacco(bedi)smoking since 30yrs 1pack/day
• Daily routine- He generally wakes up at 6:00am in the morning and at 7:00am he'll have his breakfast(rice) .And the goes for farming ,and then he'll have his lunch at 2:00pm and returns from farming at 6:00 in the evening and drinks alcohol and goes to bed around 9:00pm.
GENERAL EXAMINATION
On Examination,
patient is conscious,coherent,co - operative and well Oriented to time,place and person.
There are no signs of
Icterus,cyanosis,clubbing,Lymphadenopathy and oedema
There is presence of mild pallor.
VITALS
Temperature: 98°F
PR: 82bpm
BP:90/60
RR:18/min
RBS-541mg/dl
Sytemic examination
C VS:
No thrills
S1 and S2 +
NO murmurs
Respiratory system
NO Dyspnoea
NOWheeze
Trachea is centrally located
Abdomen
soft and non tender
NO palpable Mass
Liver and Spleen are not palpable
CNS
NAD
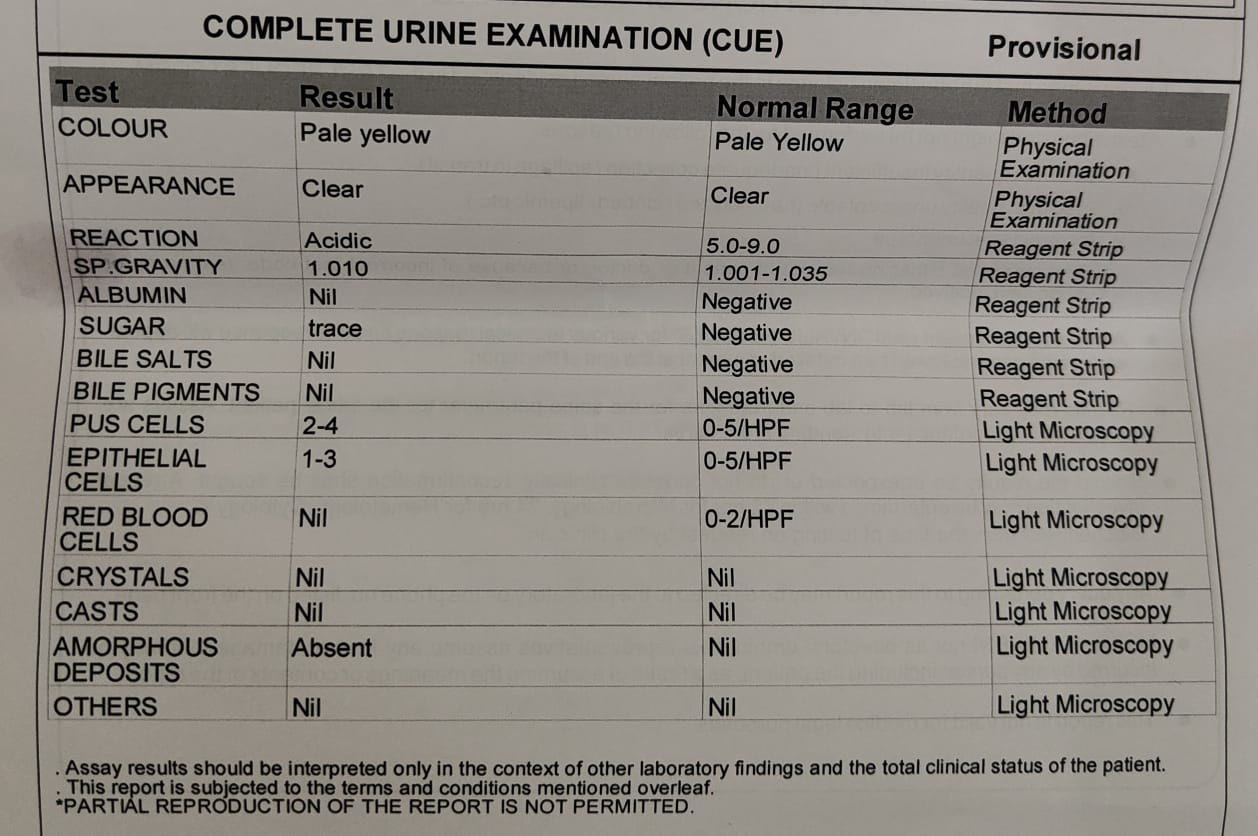
INVESTIGATIONS
DIAGNOSIS
Uncontrolled Diabetes mellitus
TREATMENT
27/7/22
• Tab.BENFOTHIAMINE PO/OD
• TAB.GLIMI -M1 PO/OD
• INJ. HAI 6units S.C
• GRBS monitoring
28/7/22
• Tab.BENFOTHIAMINE PO/OD
• TAB.GLIMI -M1 PO/OD
• INJ. HAI 6units S.C
• GRBS monitoring
29/7/22
Tab.BENFOTHIAMINE PO/BD
Tab.GLIMI-M1 PO/BD
Tab PREGABA-M 75mg
Vitals
29/07/22
BP 110/70mm Hg
PR 68/min
30/7/22
GRBS monitoring
12pm-321-HAl 4units sc
3pm - 325
7pm - 466 - Tab.Glimi 2.5mg
Tab metformin 1g/dl
12am- Hi - HAI units SC
4am - 177
31/07/22
8am - 239
1am - 348
2pm- 324
4pm-528 Glimi 4mg metformin 1g/dl
10pm-345
2am- Hi Glimi 4mg metformin 1g/dl
01/08/22
Glimi 4mg metformin 1g/dl
8am-288
10am-352
1pm-200
4pm-394
8pm-338 - Glimi 4mg metformin 1g/dl
11pm-333
2am-336
02/8/22
Glimi 4mg metformin 1g/dl
8am-155
11:30am -318
5:00pm-394
8:00pm- 338
10:30pm-477
2:00am-362
03/08/22
8:00am-135










Comments
Post a Comment